What is Brachytherapy?
Prostate brachytherapy involves the precise placement of short-range low-level radiation-material directly into the prostate gland.
This allows the prostate to be specifically treated because very little radiation penetrates outside of the prostate gland, so the treatment reduces damage to surrounding healthy tissue, thereby limiting side effects.
Radiation therapy is a safe and effective treatment for prostate cancer and is designed to destroy or injure cancer cells so they cannot multiply.
Advantages of Brachytherapy for Prostate Cancer
Prostate brachytherapy avoids major surgery and is a minimally invasive procedure.
Compared to External Beam Radiotherapy, brachytherapy requires
- Fewer visits to the hospital
- Has a shorter therapeutic duration and
- Is less likely to cause long term rectal problems or erectile dysfunction
Compared to radical prostate surgery, brachytherapy is
- Simple
- Less invasive, and
- Has a shorter recovery time and is less likely to affect urinary incontinence
Types of Brachytherapy
Brachytherapy implants are enclosed in a protective capsule or wire, which allows the ionizing radiation to escape to treat and kill surrounding tissue but prevents the charge of radioisotope from moving or dissolving in body fluids.
Brachytherapy implants can be in the form of:
- Low dose rate brachytherapy 'seeds'
- High dose rate brachytherapy
LDR Brachytherapy Seeds
Low dose rate brachytherapy or LDR brachytherapy are seeds of radioactive iodine. They are about the size of a grain of rice and are inserted into the prostate through hollow needles placed through the skin below the scrotum and near the tumour.
This procedure is generally performed under a general anaesthetic and is called a brachytherapy Implant.
Slowly over a number of months, the seeds deliver a dose of radiation to the prostate cancer
HDR Brachytherapy
High dose rate brachytherapy is based on similar principles to that of LDR brachytherapy but the delivery is a bit different.
The radioactive sources are removed from the patient at the end of each treatment session and the Iridium radiation sources deliver a more intense but short-lived dose of radiation.
Typically, HDR brachytherapy is over 3 sessions and is used for more high-risk but localised prostate cancers.
HDR brachytherapy is often given in conjunction with External Beam Radiation Therapy.
Criteria for Prostate Brachytherapy
Not all patients are suitable for brachytherapy. The guidelines that determine whether a patient is suitable for brachytherapy include the following:
- Fitness level
- Symptoms
- Prostate gland size
- Whether cancer has spread beyond the prostate, and
- The aggressive nature of the cancer cells
If brachytherapy is not suitable there are other options for managing your malignancy including
that may be more suitable.
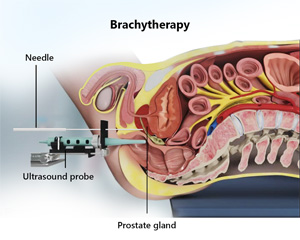
LDR Brachytherapy Procedure
The seed implants procedure usually takes approximately 2 hours and involves
- A catheter being placed in your bladder.
- An ultrasound probe is placed in your rectum to visualise the size and position of the prostate and to precisely guide position the radioactive seeds.
- A number of needles are placed between the scrotum and the anus and the seeds are placed into position.
- The needles are removed and the seeds are left within the prostate gland.
You will then be admitted to the ward and your catheter will be removed the following morning.
A postoperative CT scan will be obtained either the next day or at 1-3 months after the procedure.
The procedure involves at least one night stay at the hospital to ensure that there are no problems with urination.
After about three weeks a follow-up CT scan of the prostate allows doctors to determine the exact dose of radiation has been used.
You will then be followed up every few months when examinations and PSA tests will be done to assess how effective the treatment has been.
Follow-up tests may indicate that the brachytherapy implant has not adequately treated the gland, thus additional external beam radiation therapy would be recommended.
About the Radioactive Material
LDR uses about 80 or more seeds of radioactive iodine-125. The HDR wires contains the radioactive substance iridium.
These radioactive sources produce gamma-rays in different levels of intensity and have the same effect on cancer cells as X-rays.
Side Effects Brachytherapy Treatment for Prostate Cancer
It is important to realise that side effects may occur from all treatments.
When undergoing the procedure, you will need to undergo at least one general anaesthetic and stay in the hospital at least one night.
Some post treatments side effects can include:
- slight bleeding from the needle puncture sites
- swelling or bruising around the scrotum.
Applying an ice pack can bring relief and reduce the swelling.
Other side effects can include:
- blood in your urine after your implant, but this generally settles down within a few days.
- short or long term urinary problems such as obstruction or incontinence. This is more common in men who already have severe urinary difficulties and is why these men are excluded from brachytherapy.
- bowel irritation can occur for a few weeks after treatments, this may include frequent or loose motions and/or light bleeding from the rectum. These symptoms nearly always resolve.
Other Precautions
The level of radiation emitted by the brachytherapy seeds is very low, but as a precaution, it is advised that pregnant women and young children maintain a distance of a metre from you (except for short periods - hugs and cuddles) for the first month after the procedure.
Salvage Treatments After External Beam Radiotherapy
Salvage treatments after external beam radiotherapy, are limited in cases of cancer recurrence and are associated with high complication rates. Treatments that may be available could include:
- Radical Prostatectomy
- NanoKnife Irreversible Electroporation
- Cryotherapy
- Ultrasound Treatment (HIFU)
Complication rates of these salvage treatments can be significant. It is for these reasons that radiotherapy is generally not recommended in very young men
Complications with Brachytherapy Treatment for Prostate Cancer
Issues associated with brachytherapy treatment for prostate cancer can include:
- Impotence- approximately 22% at 1 year after the implant and is approximately 50% at 5 years. Impotence then worsens by approximately 5% per year thereafter.
- Urethral Scarring(stricture) - there is a 5% chance that scar tissue may form in the urethra. The urethra is the tube that carries urine from the bladder through the prostate and penis. It is the tube that you pass urine through in order to urinate. In these instances, the scar tissue may need to be opened with further surgery.
- Urinary frequency, pain and reduced bladder volume - there is a 1% chance of this long-term syndrome
- Pain with Urination(Dysuria), urinary urgency and frequency are approximately experienced by
- over 70% men at 3 months but typically resolves over time.
- up to 20% at 1 year
- 5% at 2 years
- 25% at 3 years, and
- 1% at 5 years.
- Retention- There is a 2 - 3% risk that you may not be able to pass urine after the procedure. This is due to swelling of the prostate gland. If this occurs, you may need to learn to pass catheters (small plastic tubes) intermittently into the bladder each time you need to pass urine. You may have to do this for some months. It is also possible that at a much later date you may require a rebore of the prostate requiring a mini-TURP Procedure to help you pass urine. There is a higher risk of incontinence associated with TURP following b
- Rectal toxicity- Up to 5% may notice an increased frequency of bowel movements and blood in the bowel motion.
- Incontinence- There is a risk that you will leak urine after the procedure. This risk is approximately 2% at about 5 years
- Fistula- There is a 1% risk that you may form an abnormal connection between the bladder and the bowel, which can result in ongoing urine infections and may require further complex surgery.
Salvage treatments after brachytherapy are limited in cases of cancer recurrence and are associated with high complication rates.
You should not father children for at least 1-2 years after the implant until all the radiation is gone.